Doctors are raising urgent concerns over a significant rise in influenza cases, with at least 1,900 deaths reported nationwide this flu season, including three children.
The Centers for Disease Control and Prevention noted that two of these children’s deaths occurred in the past week, underscoring the severity of the current outbreak.
Dr. Jocelyn Hauser, director of the DC Public Health Laboratory, explained that doctors are working intensively to test for diseases that could pose public health threats.
“The really only time that people see us is when there’s a public health emergency,” Hauser said, describing the heightened activity at public health labs across the country.
The lab receives nasal swabs from doctors’ offices and hospitals nationwide, which are then logged and sent to the CDC for analysis. This flu season has recorded at least 4.6 million cases, 49,000 hospitalizations, and 1,900 deaths in the United States alone.
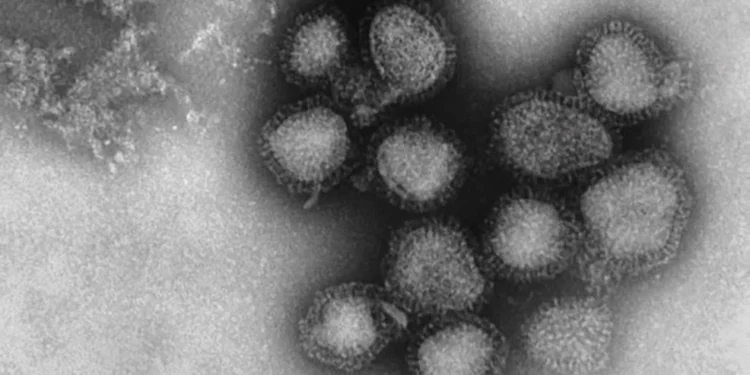
The dominant strain, subclade K, a mutation of influenza A, is driving the surge in cases.
Professor Andrew Pekosz from Johns Hopkins Bloomberg School of Public Health said the new variant appears to be evading immunity people developed from previous flu infections or vaccinations.
“We think this subclade K virus is evading population immunity, meaning more people are susceptible to infection,” Pekosz explained.
While the flu vaccine remains the best protection available, Pekosz warned that this year’s shot might not be fully effective against the dominant strain.
“It has mutations that may allow it to evade some but not all of the influenza vaccine-induced protection,” he said, though he emphasized the vaccine still provides meaningful defense.
With millions of Americans preparing to travel and gather for the holidays, experts are concerned about a potential spike in cases as people congregate in close quarters.
Children, adults 65 and older, and those with underlying medical conditions face particularly high risk of severe complications from influenza.
Medical experts urge everyone six months and older to get the flu vaccine, even this late in the season, as protection takes about two weeks to develop and flu activity typically continues into spring.
The three children’s deaths represent tragic outcomes in cases where influenza can rapidly progress to severe illness. Children’s immune systems may not respond as robustly to the virus as adults, and certain underlying conditions can increase vulnerability.
The 4.6 million cases reported likely represent a fraction of actual infections, as many people with mild flu symptoms never seek medical care or get tested. The true case count could be several times higher.
The 49,000 hospitalizations demonstrate the strain on healthcare systems already dealing with other respiratory viruses. Emergency departments and intensive care units fill quickly when flu activity surges, particularly during holiday periods when staffing may be reduced.
The subclade K mutation’s ability to evade population immunity means people who normally avoid flu infection because of residual immunity from previous exposures are getting sick this year. This expands the pool of vulnerable individuals beyond the typical high-risk groups.
The timing of the surge, coinciding with holiday travel and gatherings, creates conditions for accelerated transmission. Airports, train stations, family dinners, and holiday parties all provide opportunities for the virus to spread from infected to susceptible individuals.
The vaccine effectiveness concerns don’t mean people should skip vaccination. Even partial protection significantly reduces the risk of severe disease, hospitalization, and death. A vaccine that’s 40 percent effective still prevents hundreds of thousands of infections.
The spring projection for continued flu activity means this season could extend longer than typical years when activity peaks in January and February. An extended season means more total cases and deaths even if peak intensity doesn’t increase.